Abstract
Introduction: The gut microbiota plays an important role in maintaining intestinal homeostasis and outcomes after allogeneic hematopoietic stem cell transplantation (allo-HCT). Post-transplant loss of microbiota diversity in patients has been associated with increased infections, graft-versus-host disease (GVHD), disease relapse, and treatment-related mortality. Case studies of fecal microbiota transplantation (FMT) from healthy donors into patients with steroid-resistant gastrointestinal GVHD suggest that FMT may restore the normal microbiota and improve GVHD. However, it remains unclear what constitutes the "optimal" target microbiota and how different changes in the microbiota may impact GVHD. A particularly interesting question is whether the goal of FMT should be to replicate the original recipient microbiota (recipient FMT) or to transfer the donor microbiota (donor FMT), given that the donor microbiota may be more compatible with the transplanted donor immune system.
Methods: To test the hypothesis that donor FMT improves GVHD, we evaluated FMT in the context of our well-established allo-HCT acute GVHD model. T-cell depleted bone marrow (TCD BM) from C57BL/6 mice was transplanted into BALB/c mice without causing GVHD. T cells (1 x 106) from C57BL/6 donors were then be added back to induce GVHD. The BALB/c recipient microbiota was modified by FMT and/or antibiotics. FMT was performed by gavaging freshly collected stool from healthy mice of stem cell donor strain (B6, donor FMT) or recipient strain (BALB/c, recipient FMT). To avoid the potential mechanical injury caused by oral gavage that may affect results, we also evaluated another method of FMT in which allo-HCT recipients were housed with healthy mice, resulting in FMT via coprophagy. To test the effect of antibiotics, some recipient mice were supplied with imipenem and vancomycin in drinking water for three days before FMT. Proliferation of luciferase-labeled T cells was monitored using bioluminescent imaging.
Results:
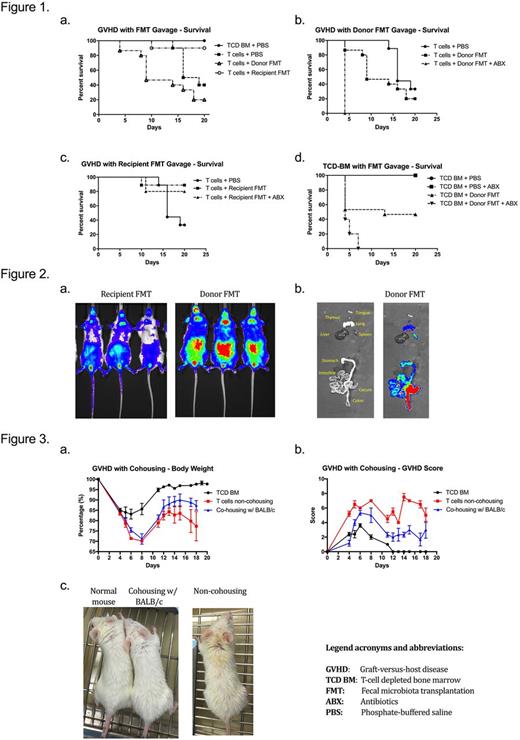
As expected, BALB/c mice receiving TCD BM from C57BL/6 had no GVHD, while BALB/c mice receiving TCD BM with 1 x 106 T cells had significant GVHD-related mortality. Contrary to our original hypothesis, donor FMT significantly worsened mortality, while recipient FMT significantly improved mortality (Fig. 1a). The addition of antibiotics particularly exacerbated early morality in the donor FMT group (Fig. 1b) while antibiotics had minimal effect in the recipient FMT setting (Fig. 1c). Interestingly, even in the context of TCD BM alone, donor FMT worsened survival, and this effect was enhanced with the addition of antibiotics (Fig. 1d). Deaths were early and consistent with infection on necropsy.
To better understand the mechanisms by which FMT affect survival, we observed T-cell proliferation using bioluminescent imaging of luciferase-labeled T cells. Mice that received recipient FMT had significantly lower luminescence in GVHD major target organs compared to the mice that received donor FMT, indicating less T-cell proliferation (Fig. 2), which is consistent with less T-cell activation and less GVHD.
Similar results were seen in co-housing experiments, in which co-housing with healthy recipient animals improved body weight and GVHD scores (Fig. 3). Preliminary 16s ribosomal RNA sequencing results support our hypothesis that FMT changes the microbiome, and these changes in the microbiome are linked to clinical outcomes. We will also explore the pathological changes in the gut microenvironment and the potential mechanism.
Conclusion: Recipient FMT in the context of allogeneic HCT helped restore the gut microbiota, suppress T-cell responses in GVHD-associated organs, and ameliorated GVHD. In contrast, donor FMT resulted in a high risk of bacterial infections as well as more severe GVHD. This study may provide crucial clinical guidance for using FMT as a potential treatment for GI GVHD.
Sung: Novartis: Research Funding; Merck: Research Funding; Cellective: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal